Cut your risk of diabetic retinopathy in half! You can when you keep your blood glucose level below 6.
This is the powerful message of a study announced at the recent annual convention of the American Diabetes Association in New Orleans. It’s published in the July 2016 issue of Diabetes Care.
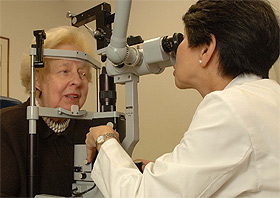
Dr. Chew Examines a Woman’s Eyes
The study also showed that one drug, a cholesterol medicine called fenofibrate, might be worth taking to control the progression of diabetic retinopathy. But the drug loses its effectiveness after people stop taking it, unlike the continued benefits from near-normal blood glucose levels below 6 after this intensive control stopped.
The new study, known as ACCORDION, is a follow-up through 2014 of the diabetic retinopathy progression of 1,310 people who participated in the ACCORD (Action to Control Cardiovascular Risk in Diabetes) study from 2003 to 2009.
Poorly controlled diabetes can lead to blindness
Diabetes is the leading cause of blindness among working-age adults in the United States, according to the National Eye Institute, which funded part of the study. The lead author, Emily Chew, MD, is the deputy director of NEI’s Division of Epidemiology and Clinical Applications.
About 7.7 million Americans now have diabetic retinopathy. One of the most disturbing facts about diabetic eye disease is that between 40 and 45 percent of Americans diagnosed with diabetes have some stage of diabetic retinopathy, although only about half are aware of it.
What stops retinopathy
The ACCORDION study evaluated 1,310 people who participated in the ACCORD study to determine what effect intensive glucose control and fenofibrate had on the progression of diabetic retinopathy. The ACCORD researchers had randomly assigned its more than 10,000 participants to intensive treatment with a target A1C of less than 6 or to the standard treatment of 7.
Other arms of the study separated participants into systolic blood pressure of less than 120 mm Hg and 140 mm Hg. But the more intensive blood pressure control had no effect. A third arm tested the results of taking 160 mg of fenofibrate plus simvastatin or placebo instead of the fenofibrate plus simvastatin.
“The treatment phase of the glycemic control portion of ACCORD had been planned to last 5.6 years, but was stopped at 3.5 years due to an increase in death among participants in the intensive glycemic control group,” notes the National Eye Institute’s press release for ACCORDION. (The full-text of study itself doesn’t mention that.)
Are hypos the problem?
Seven years ago I reported here that 257 patients in ACCORD’s intensive therapy group died, compared with 203 in the standard therapy group. In that article, I speculated that we needed to separate out the effects of the different drugs used for tight control.
Now, a retrospective analysis, “Survival in People with Type 2 Diabetes with Lower Glycosylated Hemoglobin,” 173-OR, also presented at the recent American Diabetes Association convention, lends support to the hypothesis that different drugs that people with diabetes take to get tight control make a big difference. Professor Craig Currie of the UK’s Cardiff University School of Medicine and the director of the research consultancy Pharmatelligence presented the study.
Insulin and the sulfonylureas can cause hypos
Based on an analysis of about 16 million records in the UK’s Clinical Practice Research Datalink, researchers studied what happened to people who took different diabetes drugs, including those like metformin that have a low risk of hypoglycemia, or hypos, as well as insulin and the sulfonylureas, which include glimepiride (Amaryl), glipizide (Glucotrol and Glucotrol XL), and glyburide. Then they looked at the risk of death of those who had an A1C level of less than 7, comparing that with the risks at higher A1C levels.
They concluded that the increased risk was “mainly driven by therapies known to cause hypoglycemia.” They presented data showing that these therapies are insulin and the sulfonylureas.
After his talk, I asked Professor Currie if he could say anything about the mortality with a very low-carb diet to achieve a low A1C without taking any drugs, which is my own treatment strategy. They haven’t done the analysis yet, but “we have loads of data in people being managed with diet and exercise,” Professor Currie told me. “It’s possible to do it, and it’s a good suggestion.”
Tight control still matters
It’s appears increasingly likely that hypos rather than tight control are the main reason for the disturbing ACCORD findings. “The take-home is that glycemic control still matters for Type 2,” Dr. Chew says.
“I always tell my patients, ‘No drug can do as much as tight glycemic control.’ It’s a mystery, but it works.”
This article is based on an earlier version of my article published by HealthCentral.
Never Miss An Update
Subscribe to my free newsletter “Diabetes Update”
I send out my newsletter on first of every month. It covers new articles and columns that I have written and important developments in diabetes generally that you may have missed.

